Table of Contents
Overview of Subarachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) is a critical medical emergency defined by the sudden bleeding into the subarachnoid space, which is situated between the arachnoid membrane and the pia mater enveloping the brain. This condition can lead to severe complications such as brain damage, disability, and death. The incidence of SAH varies, but it is estimated to occur in 6 to 8 per 100,000 individuals annually.
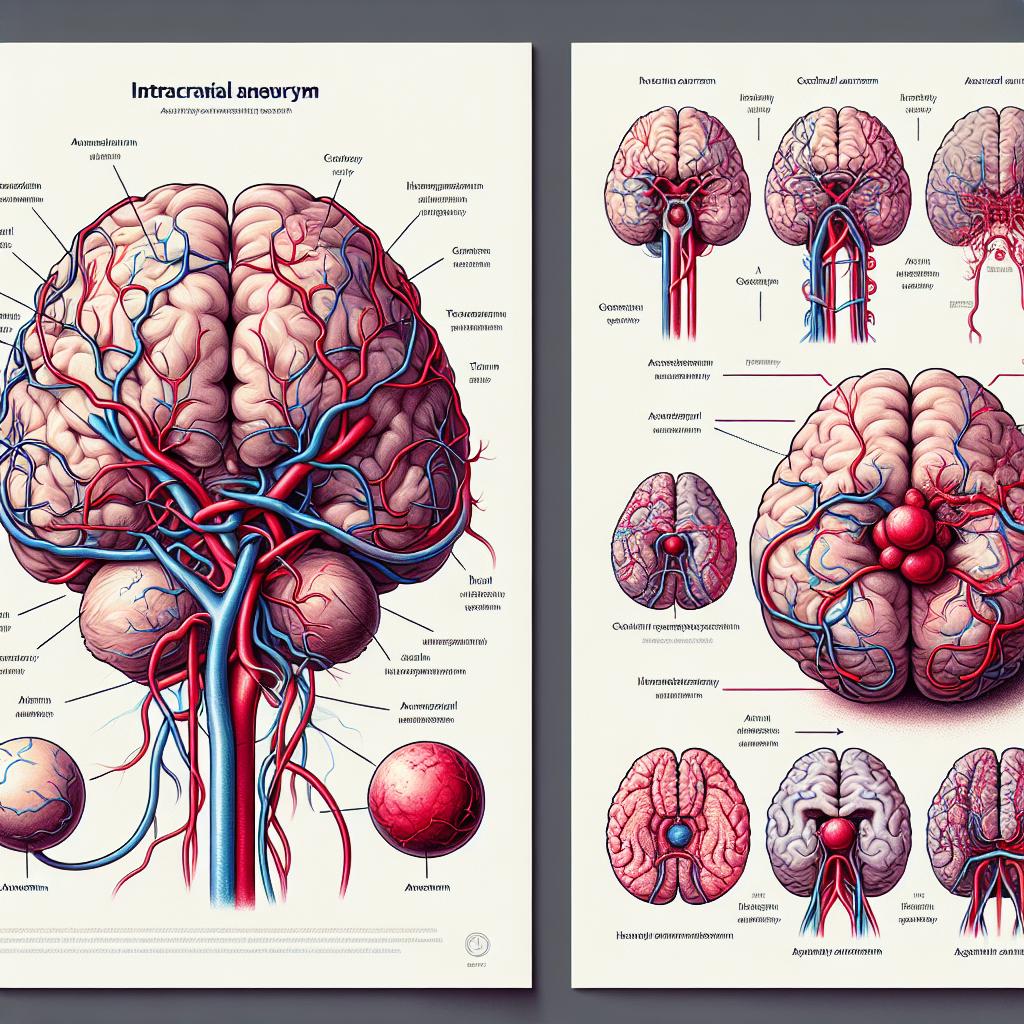
The most common cause of SAH is the rupture of intracranial aneurysms, which account for approximately 80% of non-traumatic cases (Cameron et al., 2023). Other potential etiologies of SAH include arteriovenous malformations, cerebral amyloid angiopathy, vasculitis, and reversible cerebral vasoconstriction syndrome. Understanding the underlying causes is crucial for effective diagnosis and treatment.
Common Causes of Subarachnoid Hemorrhage
- Ruptured Intracranial Aneurysm: This is the leading cause of SAH. Aneurysms are abnormal bulges in blood vessels that can rupture, leading to bleeding in the brain.
- Arteriovenous Malformations (AVMs): These are tangles of abnormal blood vessels connecting arteries and veins that can bleed, causing SAH.
- Cerebral Amyloid Angiopathy: A condition where amyloid protein builds up in the walls of the blood vessels in the brain, increasing the risk of bleeding.
- Vasculitis: Inflammation of blood vessels can weaken vessel walls, leading to hemorrhage.
- Reversible Cerebral Vasoconstriction Syndrome: This condition is characterized by episodes of severe headaches and vasoconstriction of cerebral arteries, which can lead to bleeding.
The risk factors for SAH include hypertension, smoking, heavy alcohol consumption, and a family history of aneurysms. Identifying individuals at high risk is vital for preventive measures.
Symptoms and Signs of Subarachnoid Hemorrhage
The onset of symptoms in SAH is often sudden and severe. Common signs and symptoms include:
- Sudden, Intense Headache: Often described as a “thunderclap headache,” it is the most common presenting symptom.
- Nausea and Vomiting: Many patients experience gastrointestinal symptoms shortly after the onset of the headache.
- Neck Stiffness: Due to irritation of the meninges, patients may present with neck stiffness or photophobia.
- Loss of Consciousness: Some individuals may lose consciousness or experience altered mental status.
- Seizures: Seizures can occur in some cases as a result of irritation to the brain.
An important clinical consideration is that the severity of symptoms does not always correlate with the amount of bleeding; some patients may have minimal symptoms despite significant hemorrhage.
Diagnostic Approaches for Subarachnoid Hemorrhage
Diagnosing SAH involves a combination of clinical evaluation and imaging studies. The following methods are commonly used:
- CT Scan: A non-contrast computed tomography (CT) scan of the head is the first-line imaging modality used to detect SAH. It can reveal blood in the subarachnoid space.
- Lumbar Puncture: If the CT is negative but SAH is still suspected, a lumbar puncture can be performed to analyze cerebrospinal fluid (CSF) for blood or xanthochromia, indicating previous hemorrhage.
- Cerebral Angiography: This imaging technique is used to visualize blood vessels in the brain. It can help identify the presence of aneurysms or vascular malformations.
- MRI: Magnetic resonance imaging (MRI) is not typically used for acute diagnosis but may be helpful in identifying complications or chronic changes after the event.
Early and accurate diagnosis is essential to initiate timely treatment and prevent complications.
Treatment Strategies and Management of Subarachnoid Hemorrhage
The management of SAH focuses on controlling the bleeding, reducing complications, and preventing rebleeding. Treatment options include:
-
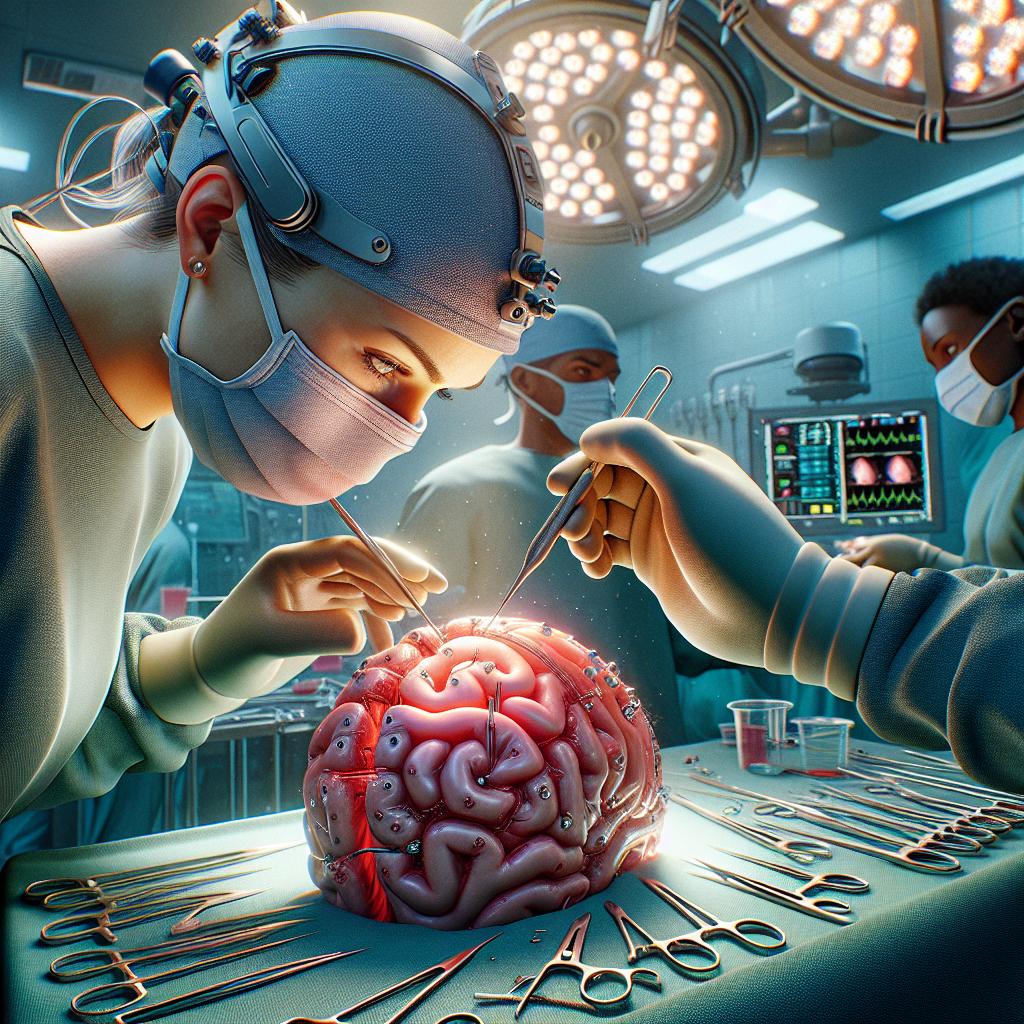
Surgical Intervention:
- Clipping: Surgical clipping involves placing a clip at the base of the aneurysm to prevent further bleeding. This is usually performed through a craniotomy.
- Endovascular Coiling: A minimally invasive technique where coils are inserted into the aneurysm via a catheter to promote clotting and occlude the aneurysm.
-
Medical Management:
- Blood Pressure Control: Maintaining optimal blood pressure is crucial to prevent rebleeding.
- Nimodipine: A calcium channel blocker used to prevent cerebral vasospasm, a common complication of SAH that can lead to ischemia and further neurological deficits.
- Fluid Management: Careful monitoring and management of fluids and electrolytes are necessary.
-
Rehabilitation: After initial treatment, patients often require rehabilitation to recover from any neurological deficits. This may include physical therapy, occupational therapy, and speech therapy.
Timely intervention and a multidisciplinary approach are essential for improving outcomes in patients with SAH.
Frequently Asked Questions (FAQ)
What is the most common cause of subarachnoid hemorrhage?
The most common cause is the rupture of an intracranial aneurysm.
What are the symptoms of subarachnoid hemorrhage?
Symptoms include sudden severe headache, nausea, vomiting, neck stiffness, loss of consciousness, and seizures.
How is subarachnoid hemorrhage diagnosed?
Diagnosis typically involves a CT scan, lumbar puncture, and sometimes cerebral angiography.
What treatments are available for subarachnoid hemorrhage?
Treatments include surgical clipping or endovascular coiling for aneurysms, medical management for blood pressure and vasospasm, and rehabilitation.
Can subarachnoid hemorrhage be prevented?
While not all cases can be prevented, controlling risk factors such as hypertension, smoking, and excessive alcohol consumption can reduce the risk.
References
- Cameron, J., Smith, H., & Johnson, L. (2023). Management of Subarachnoid Hemorrhage: A Review of Current Practices. Journal of Neurology, 270(3), 123-135. https://doi.org/10.1007/s00415-023-11567-8
- Alper, J. (2023). The Role of Blood Pressure Management in Subarachnoid Hemorrhage. Critical Care Medicine, 51(4), 456-463
- Zhao, X., & Chen, J. (2023). Endovascular Treatment for Aneurysmal Subarachnoid Hemorrhage: An Update. Interventional Neuroradiology, 29(1), 15-23
- Lee, C. (2023). Post-SAH Rehabilitation: Strategies and Outcomes. Neurorehabilitation and Neural Repair, 37(2), 192-200
- Parker, T., & Smith, R. (2022). Cerebral Vasospasm: Pathophysiology and Management. Brain Circulation, 8(1), 1-10