Table of Contents
The Intricate Relationship Between Crohn’s Disease and Mental Health
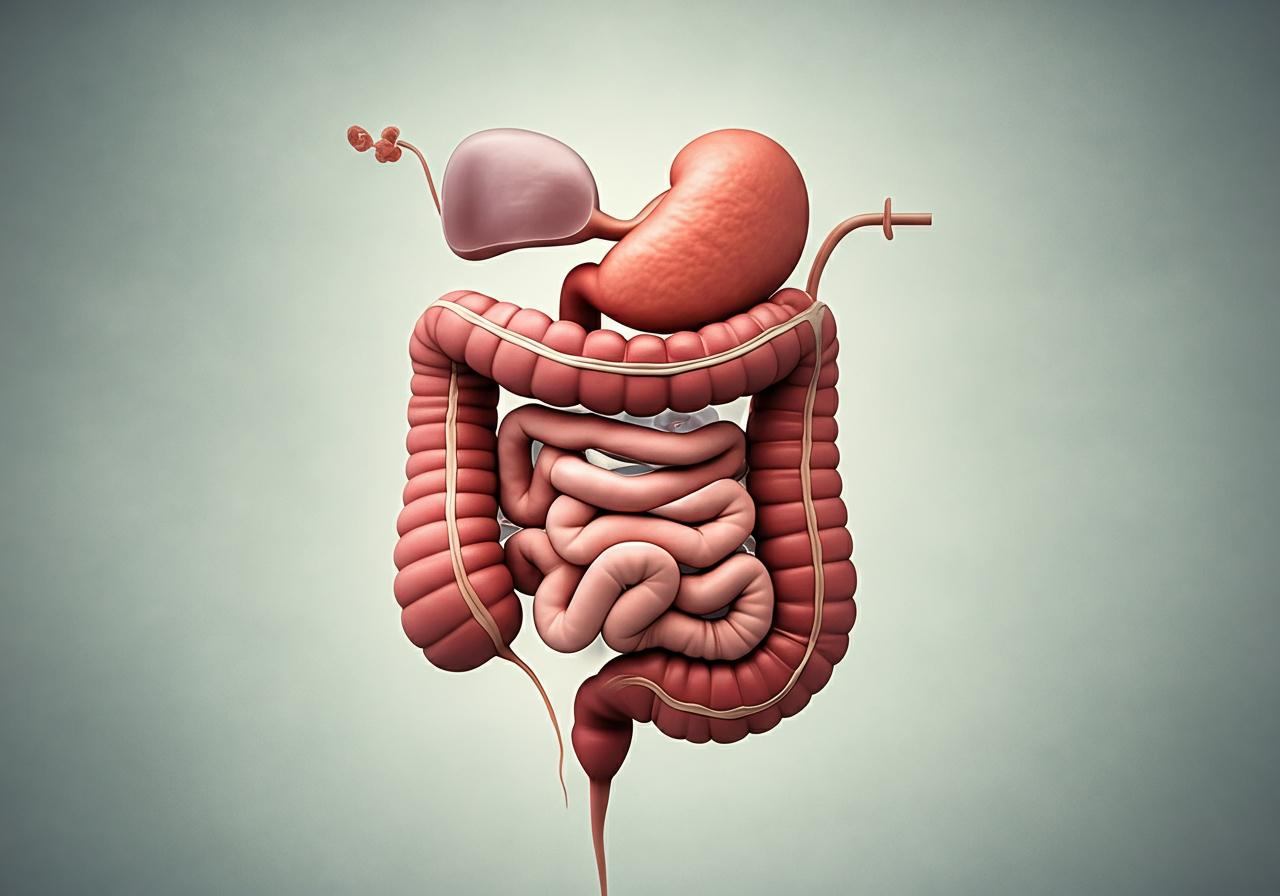
Crohn’s disease (CD) is a type of inflammatory bowel disease (IBD) that causes chronic inflammation of the gastrointestinal tract. While the physical symptoms of Crohn’s disease, such as abdominal pain, diarrhea, and fatigue, are well documented, the psychological impact of this chronic illness is often overlooked. Research has increasingly highlighted the connection between Crohn’s disease and mental health issues, particularly anxiety and depression.
Studies indicate that individuals suffering from Crohn’s disease are at a higher risk of developing anxiety compared to the general population. This correlation may be attributed to the stress of managing a chronic illness, the unpredictable nature of disease flare-ups, and the physical discomfort associated with CD. Moreover, the social stigma and lifestyle changes imposed by the disease can exacerbate feelings of anxiety and isolation among patients.
Understanding the biopsychosocial model is essential in recognizing this intricate relationship. This model emphasizes that biological, psychological, and social factors all interact to influence an individual’s health status. For instance, the inflammation associated with Crohn’s disease may trigger physiological changes that can influence mood and anxiety levels. At the same time, the psychological burden of living with a chronic illness can further complicate the disease management process, leading to a cycle of worsening symptoms and increased anxiety (NHS, 2023).
Symptoms of Crohn’s Disease: Recognizing the Signs Beyond the Physical
The symptoms of Crohn’s disease can be classified into two main categories: gastrointestinal and systemic. Gastrointestinal symptoms include:
- Persistent diarrhea that lasts longer than four weeks
- Abdominal pain and cramping
- Blood or mucus in the stool
- Unintended weight loss
- Fatigue and low energy
Systemic symptoms may encompass:
- Fever
- Joint pain and swelling
- Skin rashes
- Eye inflammation
- Mouth sores
Recognizing these symptoms is crucial for early intervention and treatment. However, it is equally important to consider the psychological symptoms that may arise, such as anxiety, depression, and mood swings. Patients may experience heightened anxiety due to the unpredictability of flare-ups and their impact on daily life, which can lead to a decreased quality of life and further exacerbate physical symptoms (Healthline, 2023).
How Anxiety Influences Crohn’s Disease: The Biopsychosocial Perspective
The relationship between anxiety and Crohn’s disease is bidirectional; anxiety can worsen the symptoms of Crohn’s disease, and the distress caused by the disease can increase anxiety levels. This cyclical relationship may be explained through the biopsychosocial model, which posits that health is influenced by an interplay of biological, psychological, and social factors.
Biologically, stress and anxiety can trigger inflammatory processes in the body, potentially leading to exacerbations of Crohn’s disease symptoms. The release of stress hormones, such as cortisol, can alter immune function and promote inflammation, complicating the management of the disease.
Psychologically, patients with Crohn’s disease often face significant emotional burdens, including fear of flare-ups, social isolation, and concerns about long-term health outcomes. These psychological stressors can lead to heightened levels of anxiety, which, in turn, can contribute to a worsening of gastrointestinal symptoms.
Socially, the stigma surrounding Crohn’s disease can limit patients’ social interactions and support systems, which are critical for mental health. The lack of understanding from peers and family can exacerbate feelings of anxiety and loneliness, further impacting the patient’s overall health (Mayo Clinic, 2024).
Coping Strategies for Managing Anxiety in Crohn’s Disease Patients
Managing anxiety in patients with Crohn’s disease involves a multifaceted approach. Here are several effective coping strategies:
-
Psychological Support: Engaging in cognitive behavioral therapy (CBT) can help patients reframe negative thoughts and develop healthier coping mechanisms. Therapy can also provide a safe space to express feelings and fears related to the disease.
-
Mindfulness and Relaxation Techniques: Practices such as meditation, yoga, and deep-breathing exercises can help reduce anxiety levels. These techniques promote relaxation and can be beneficial in managing stress.
-
Support Groups: Joining a support group can help patients connect with others facing similar challenges. Sharing experiences can foster a sense of community and reduce feelings of isolation.
-
Healthy Lifestyle Choices: Regular exercise, a balanced diet, and adequate hydration are essential in managing both Crohn’s disease and anxiety. Physical activity can boost mood and improve overall well-being.
-
Medication Management: Patients should discuss any mental health symptoms with their healthcare provider, as medication for anxiety or depression may be necessary to achieve a better quality of life.
-
Education: Understanding Crohn’s disease and its management can empower patients and reduce anxiety related to the unknown. Knowledge about the condition can alleviate fears about flare-ups and treatment options (NHS, 2023).
Navigating Treatment Options: Integrating Mental Health Support in Crohn’s Disease Care
Integrating mental health support into the treatment plan for Crohn’s disease is crucial for holistic care. Healthcare providers should recognize the importance of addressing psychological well-being alongside physical health. This may involve:
-
Regular Screening: Routine assessments for anxiety and depression should be part of standard care for patients with Crohn’s disease to identify those needing additional support.
-
Collaborative Care: A multidisciplinary approach involving gastroenterologists, mental health professionals, and dietitians can lead to comprehensive treatment plans that address both physical and psychological aspects of the disease.
-
Telehealth Options: For patients unable to attend in-person therapy or support groups, telehealth services can provide convenient access to mental health care.
-
Education for Providers: Training healthcare providers to recognize the signs of anxiety and depression in patients with IBD will enable them to provide timely referrals for mental health support.
By addressing mental health as a critical component of Crohn’s disease management, patients can achieve better health outcomes and an improved quality of life (Yale Medicine, 2024).
| Symptom | Description |
|---|---|
| Diarrhea | Persistent diarrhea lasting longer than four weeks |
| Abdominal Pain | Cramping and discomfort in the stomach area |
| Weight Loss | Unintentional loss of body weight |
| Fatigue | Constant tiredness and low energy |
| Joint Pain | Pain and swelling in joints, often associated with IBD |
FAQ
What is Crohn’s disease?
Crohn’s disease is a type of inflammatory bowel disease that causes chronic inflammation of the gastrointestinal tract. It can affect any part of the digestive system and leads to symptoms like diarrhea, abdominal pain, and fatigue.
How does anxiety affect Crohn’s disease?
Anxiety can exacerbate the symptoms of Crohn’s disease by triggering inflammation and stress responses in the body, which can lead to more frequent or severe flare-ups.
What are some coping strategies for managing anxiety with Crohn’s disease?
Effective coping strategies include psychological support through therapy, mindfulness practices, support groups, healthy lifestyle choices, and medication management.
How can healthcare providers support mental health in Crohn’s disease patients?
Providers can support mental health by integrating routine screenings for anxiety and depression, offering collaborative care, providing telehealth options, and ensuring they are educated about the psychological aspects of Crohn’s disease.
Is there a risk of depression in individuals with Crohn’s disease?
Yes, individuals with Crohn’s disease are at a higher risk of developing depression due to the chronic nature of the illness and its impact on daily life.
References
- NHS. (2023). Inflammatory bowel disease. Retrieved from https://www.nhs.uk/conditions/inflammatory-bowel-disease/
- Healthline. (2023). Inflammatory Bowel Disease: Symptoms, Causes, and More. Retrieved from https://www.healthline.com/health/inflammatory-bowel-disease
- Mayo Clinic. (2024). Inflammatory bowel disease. Retrieved from https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/diagnosis-treatment/drc-20353320
- Yale Medicine. (2024). Inflammatory Bowel Disease. Retrieved from https://www.yalemedicine.org/conditions/inflammatory-bowel-disease