Table of Contents
What Is Lucentis? An Overview of Its Purpose and Importance

Lucentis, known generically as ranibizumab, is a medication widely used in the treatment of various eye conditions, particularly those involving abnormal blood vessel growth and leakage in the retina. As a member of the anti-vascular endothelial growth factor (anti-VEGF) drug class, it plays a crucial role in managing diseases such as wet age-related macular degeneration (AMD), diabetic macular edema (DME), and retinal vein occlusion (RVO). These conditions can lead to significant vision impairment and even blindness if not properly treated.
The importance of Lucentis lies in its ability to inhibit VEGF, a protein that promotes the growth of new blood vessels. In conditions like wet AMD, excess VEGF leads to the formation of leaky and abnormal blood vessels in the eye, causing fluid accumulation and retinal damage. By blocking this protein, Lucentis helps reduce swelling, stabilize vision, and maintain the integrity of the retinal structure.
According to recent studies, properly administered Lucentis can improve visual acuity in many patients, making it a fundamental component of contemporary ophthalmic care (Lucentis dosage: Form, strengths, how it’s given, and more, 2023).
The Forms and Strengths of Lucentis: What You Need to Know
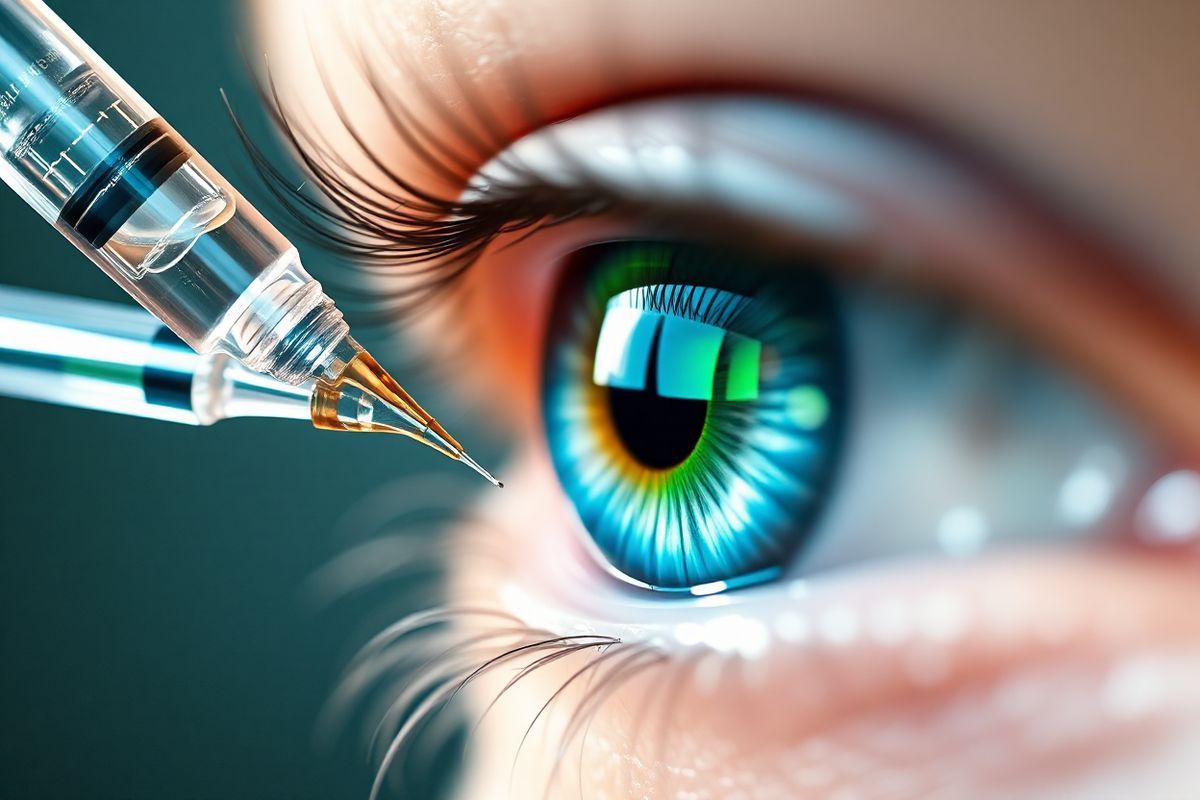
Lucentis is available as a liquid solution in prefilled syringes, specifically designed for intravitreal injection, which means it is injected directly into the vitreous cavity of the eye. This method of administration allows for rapid delivery of the medication to the target area, enhancing its effectiveness.
The drug comes in two strengths:
- 0.3 mg in 0.05 mL (a concentration of 6 mg/mL)
- 0.5 mg in 0.05 mL (a concentration of 10 mg/mL)
These strengths allow ophthalmologists to tailor the treatment according to the specific needs of the patient and the severity of the eye condition being treated. For example, for diabetic macular edema and diabetic retinopathy, the standard dosage is typically 0.3 mg, whereas for wet AMD and macular edema following retinal vein occlusion, the usual dosage is 0.5 mg (Lucentis dosage: Form, strengths, how it’s given, and more, 2023).
Typical Dosages for Lucentis: Tailoring Treatment to Eye Conditions
The specific dosage of Lucentis is determined based on the condition being treated. Here’s a breakdown of typical dosages:
| Condition | Dosage | Frequency |
|---|---|---|
| Wet Age-Related Macular degeneration (AMD) | 0.5 mg/0.05 mL | Every 28 days (once monthly) |
| Macular Edema Following Retinal Vein Occlusion | 0.5 mg/0.05 mL | Every 28 days (once monthly) |
| Diabetic Macular Edema | 0.3 mg/0.05 mL | Every 28 days (once monthly) |
| Diabetic retinopathy | 0.3 mg/0.05 mL | Every 28 days (once monthly) |
| Myopic Choroidal Neovascularization | 0.5 mg/0.05 mL | Every 28 days for up to 3 months |
For wet AMD, an initial treatment phase may involve monthly injections, which can later be adjusted based on the patient’s response and the results of regular eye examinations. The effectiveness of Lucentis in maintaining visual acuity has been well-documented, indicating that adherence to the recommended schedule is critical for optimal outcomes (Lucentis dosage: Form, strengths, how it’s given, and more, 2023).
How Are Lucentis Injections Administered? A Step-by-Step Guide
The administration of Lucentis injections is a straightforward yet precise procedure performed by an ophthalmologist. Below is a step-by-step guide on how these injections are typically given:
-
Preparation: The patient is usually reclined in a comfortable chair. The eye undergoing treatment is numbed using anesthetic eye drops or gel. This minimizes discomfort during the injection.
-
Cleaning the Eye: An antiseptic solution, typically povidone-iodine, is applied to the eye and surrounding areas to reduce the risk of infection.
-
Using a Speculum: An eyelid speculum may be used to gently hold the eyelids open, ensuring the doctor has a clear view of the eye and preventing blinking during the procedure.
-
Positioning: The ophthalmologist may ask the patient to look in a specific direction to allow access to the appropriate area of the eye for the injection.
-
Injection: A fine needle is carefully inserted through the white part of the eye (the sclera) into the vitreous cavity. The injection itself is quick, with the medication delivered directly into the eye.
-
Post-Injection Care: After administering the injection, the ophthalmologist will clean the eye again and check for any immediate complications. The entire process usually takes about 10 to 15 minutes, although the patient should expect to be in the clinic for a longer duration due to preparatory steps and post-injection monitoring (The American Society of Retina Specialists, n.d.).
-
Follow-Up: Patients are typically monitored for any side effects or complications, and follow-up appointments are scheduled based on individual treatment plans.
The Long-Term Journey with Lucentis: What to Expect from Eye Injections
Receiving Lucentis injections is often a long-term commitment, particularly for chronic conditions like wet AMD and diabetic macular edema. The frequency of injections may vary based on the individual’s response to treatment. Initially, patients may require monthly injections, but some may eventually transition to less frequent dosing after the initial treatment phase, contingent upon their eye health and the stability of their condition (An End to Eye Injections?, 2022).
What to Expect After Injections
Following an injection, patients may experience minor side effects, including:
- Mild discomfort or irritation in the injected eye
- Temporary blurred vision
- A small amount of bleeding or a subconjunctival hemorrhage (a red spot on the white of the eye) at the injection site
Most of these side effects resolve quickly. However, patients should be vigilant for any signs of complications, such as increased pain, sudden vision changes, or persistent redness, and report these to their eye care provider promptly (Questions about injections, n.d.).
Long-Term Efficacy and Safety
Research shows that many patients can maintain or improve their vision with long-term treatment using Lucentis. Some studies suggest that a subset of patients may even be able to stop injections without losing vision, although this requires careful monitoring and evaluation by their ophthalmologist (An End to Eye Injections?, 2022).
FAQ
What conditions can Lucentis treat?
Lucentis is primarily used to treat wet age-related macular degeneration, diabetic macular edema, diabetic retinopathy, and macular edema following retinal vein occlusion.
How often will I need to receive Lucentis injections?
Initially, most patients receive injections once a month, but this can be adjusted based on individual responses and eye health.
Are there any side effects associated with Lucentis injections?
Common side effects include mild discomfort, temporary blurred vision, and subconjunctival hemorrhage. Serious complications are rare but can occur.
Can I stop getting Lucentis injections?
Some patients may be able to stop injections if their condition stabilizes, but this decision should only be made in consultation with an ophthalmologist.
What should I do if I experience pain or vision changes after an injection?
Contact your ophthalmologist immediately if you experience worsening vision, increased pain, or other unusual symptoms following an injection.
References
- Lucentis dosage: Form, strengths, how it’s given, and more. (2023). Retrieved from https://www.medicalnewstoday.com/articles/lucentis-dosage
- An End to Eye Injections? (2022). Retrieved from https://www.hopkinsmedicine.org/news/articles/2022/06/an-end-to-eye-injections
- The American Society of Retina Specialists. (n.d.). Retrieved from https://www.asrs.org/patients/retinal-diseases/33/intravitreal-injections
- Questions about injections. (n.d.). Retrieved from https://www.macularsociety.org/support/one-to-one/treatment-buddies/questions-about-injections/











